SLIPPED DISC – Is it really???
 The terms “Slipped Disc” and “Sciatica” are often used when referring to lower back pain. As a result there is a bit of confusion as to treatment options and expectations when it comes to these often painful conditions. We’ll try and help explain what they really mean.
The terms “Slipped Disc” and “Sciatica” are often used when referring to lower back pain. As a result there is a bit of confusion as to treatment options and expectations when it comes to these often painful conditions. We’ll try and help explain what they really mean.
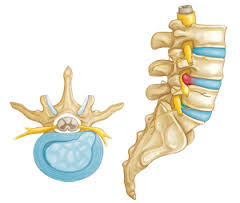
The Discs are a shock absorber which act as a spacer between each vertebra throughout our entire spine. The outer ring is known as the Disc Annulus and is like a thick rubber ring made of strong fibrous material. It contains the inside of the disc known as the nucleus. This nucleus has the consistency of jelly or toothpaste which becomes drier and more granular as we get older.
It is common to develop a bulge in the back of the disc annulus, especially over the age of 30yrs and after years of bending, sitting and heavy lifting. These bulges commonly occur in the lower back. They usually don’t cause pain until they start bumping or irritating the nerves or pain sensitive structures in that area of the spine.
Heavy lifting, excessive twisting in a bent position or something as simple as coughing or sneezing while bent forward is enough to cause the annulus to tear. This can result in deep, sharp back pain and spasm of the surrounding muscles as they try and protect the damaged areas. This is known as an annular tear or disc rupture.
If the nucleus or inside of the disc squeezes out of the disc, it can exert pressure onto the spinal cord or nerves on either side as they leave the spine. This is called Disc Protrusion, Herniation or Prolapse. This disc material can cause a chemical irritation of the nerves and surrounding tissues causing pain to be referred into the leg down the path of that nerve. The sciatic nerve runs down the back of the leg often to the outside calf and ankle hence the term sciatica.
Your physiotherapist can often identify which specific level of disc is affected depending on the path of the sciatic pain. If pressure on the nerve is large or remains constant other symptoms such as numbness, pins and needles, weakness or loss of reflexes can occur.
Disc Ruptures , Prolapses/Protrusions/Herniations or whatever you choose to call them are often very painful and debilitating, with spasm enough to prevent the patient from walking, standing or even rolling over, and pain levels causing nausea and even feinting. Fortunately, despite their incredible pain and loss of function, most of these are treatable and can resolve with the correct education, management, exercises and manual therapy. Contrary to popular belief these “Slipped Discs” cannot be suddenly popped back into place by spinal manipulation or adjustments. These techniques may be useful later on to restore better movement in the joints around the damaged disc, but if used too early can exacerbate the disc damage itself.
Physiotherapists are trained to assess the extent of damage, and will work together with your GP if further CT or MRI scans are required and to discuss the correct combination of medications. Some cases may require cortisone injections or referral to a specialist. Fortunately only a small number of these cases end up requiring surgery which is aimed at taking the disc pressure off the nerve and predominantly easing the sciatic symptoms.
There are many other causes of lower back pain which are not as extreme or debilitating as the discogenic injuries. These are treated differently by Physiotherapists and often resolve more quickly with the correct treatment and advise. Once again it comes down to being given the correct diagnosis to avoid potential minor disc injuries being made worse.
A true disc injury can take 3-6 mths to heal, and sometimes up to 12 mths to get back to full function. Clinical Pilates , Posture correction therapy and a guided rehabilitation exercise program are all very important in preventing recurrence and getting back into life’s activities. Your MGS Physiotherapist can help you from early injury and guide you through to complete recovery as needed.
